[toc]As a compound of two Greek words, the “pro” means promotion and “biotic” means life.
With a feel-good name like that, it’s no wonder they’re dominating the supplement aisle. Aside from natural sources like yogurt and sauerkraut, they’re even being added to foods like protein bars, tortilla chips, and even cookies.
Such ubiquity may be a mistake.
Are probiotics good for you?
As a dietary supplement, probiotics are marketed for the prevention of gas and bloating, regular bowel movements, and the prevention of some intestinal disorders. Overall, the customer base is heavily skewed female, which is why you typically women used for commercials and advertising.
For both women and men, it is true that these living microorganisms appear to offer health benefits for many. While not conclusively proven, there is a vast amount of research which suggests that probiotic supplements work, particularly those containing Lactobacillus and/or Bifidobacterium strains of bacteria. Human clinical evidence has suggested potential benefits for:
- Flatulence
- Diarrhea caused by infections
- Antibiotic-associated diarrhea
- Irritable bowel syndrome (IBS)
- Crohn’s disease
- Ulcerative colitis
- Stomach ulcers caused by H. pylori bacteria
- Urinary tract infections (UTI)
- Vaginal infections
- Tooth decay
- Colectomy-induced inflammation (pouchitis)
- Common colds
- Eczema
These suspected advantages are even discussed on the US government’s NIH website about probiotics. Though to reiterate, while these uses do have some clinical data to back them, there isn’t enough to classify the benefits as proven. In some cases, they may actually worsen the disease or condition they’re aimed at helping. (1) (2)
Weight loss has also been observed, particularly with Lactobacillus probiotics. In a double-blind and placebo controlled trial involving 125 obese men and women, those using Lactobacillus rhamnosus supplements had statistically significant improvements in body weight and fat mass after 24 weeks. (3)
The bias in the science
They may be small potatoes compared to prescription drugs, but make no mistake about it, these things to keep your gut healthy are big business.
Activia alone is a multi-billion dollar brand. You may recall the early days, when Jamie Lee Curtis was essentially having a poop party on TV to peddle the product.
The industry as a whole is around $40 billion per year. It’s projected that sales of probiotics will hit $64.6 billion by 2023. (4)
Whenever there’s that much money on the line, you can bet Madison Avenue is keeping a tight grip on what you know… and what you don’t.
For example, no one tells you that Lactobacillus reuteri might make you fat.
It’s used as a growth promoter in baby piglets to boost their weight. Human research has also found it to correlate with weight gain. (5)
Many – perhaps even most – probiotic supplements contain the L. reuteri strain. Nature’s Way even sells a product called Reuteri Pearls.
As discussed in the European Journal of Epidemiology, we probably aren’t hearing about all the possible reasons why probiotics are bad for you because they are being underreported. In summary, two reasons for this are:
1. Conflicts of interest with manufacturers
Many studies are financially backed by food and supplement companies. In order to please them, a study may be designed in a way that gives a ‘glass half-fill’ outcome. They may gloss over or simply not report the negative results. A study with a bad outcome may never be published, as if it never even took place.
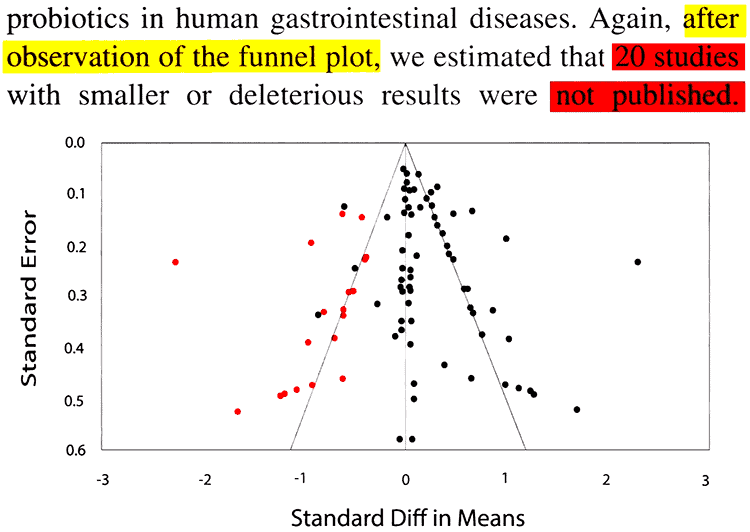
This journal article featured a meta-analysis, which is basically a pooling of results from different studies, and then analyzing them as a whole. Based on this and some fancy statistics, they determined that an estimated 20 studies on probiotics in human gastrointestinal diseases were not published:
The ones in red are believed to be missing. You and your doctor may only be seeing the studies the industry wants you to see.
Unlike pharma, where there are strict rules about disclosures of who’s funding a given study, it’s different with supplements.
“In conclusion, as for pharmaceutical industry it is clear that there are publication biases in probiotics related papers. Very commonly conflicts of interest are not reported, even when authors are directly sponsored by food industry.”
2. Preconceived notions by researchers
If the researcher leading a given study is already enthusiastic about probiotics to begin with, this may influence what they report.
“In humans the investigator hypothesis and the sponsor interest were both in favor of a probiotic effect on digestive diseases that may have led to the unreport of opposite results.”
After the journal published this, of course it got flak from those in the industry, as they tried to argue against the allegations. Isn’t that to be expected? (6)
Side effects of probiotics
- Increased gas and bloating
- Stomach ache
- Diarrhea
- Weight gain
- Increased risk of infection
- Sepsis and overstimulation of the immune system
- Interactions with antibiotics and autoimmune drugs
- Small intestinal bacterial overgrowth (SIBO)
- Increased risk of death during pancreatitis
- Gene transfer (gene movement between organisms)
- Unknown safety during pregnancy
- Unknown safety while breastfeeding

Whether probiotics will make you gain weight or lose weight is not black and white.
In horses, pigs, and livestock, there are certain strains associated with weight gain and are given for that very purpose. Human data is limited, as only Lactobacillus reuteri has been associated with obesity. The opposite has been seen with Lactobacillus rhamnosus.
Sepsis can be a life-threatening response by your body to fight an infection. It’s basically your immune system going into overdrive.
In immunodeficient mice, the side effect of sepsis was seen with human isolates of L. reuteri, L. acidophilus, and Bifidobacterium animalis or LGG. There were deaths reported with neonatal mice, which would make sense since their immune systems are less developed than the adults. (7)
The same holds true for neonatal human babies, as they are more susceptible to infection.
People with HIV and other immune system problems might also be at increased risk of sepsis being triggered by probiotic usage. The good news is that preliminary research on HIV patients suggests this is unlikely and probiotics might actually benefit this disease. (8)
There are dozens of human case studies published here there was bacterial or fungal sepsis temporarily related to probiotic supplements. This is potential danger you just don’t hear about. (9)
While sepsis is a severe overstimulation of the immune system, any amount of overstimulation may worsen autoimmune diseases such as rheumatoid arthritis, lupus, Celiac disease, multiple sclerosis (MS), plaque psoriasis, inflammatory bowel disease (IBD) and others. This is why many medications used to treat these diseases are designed to intentionally suppress the immune system.
If they are leading to an overstimulation of the immune system, probiotics might interfere with medications for autoimmune diseases.
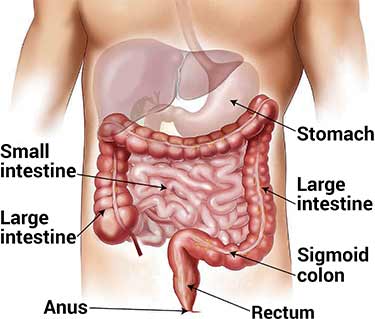
In other words, bacteria are too high up in your digestive tract.
This happens when they migrate up from your large intestine (where they belong) and grow in the small intestine (where they don’t belong). This leads to increased fermentation by the bacteria, as they munch away on the carbs/sugars while are still present in the small intestine. This can result in the side effects of excess flatulence, stomach pain, and in severe cases, malnutrition.
The problem with probiotic supplements is that they first must pass through the stomach and small intestine, before getting to the large intestine (colon).
The problem with taking probiotic supplements for SIBO is that they are entering your body orally. That means they first have to pass through where they do not belong to get to where they do belong.
The vast majority of friendly bacteria should reside in your colon. (10) (11)
If you have SIBO, chronic intestinal pseudo-obstruction (CIP) or another condition where your digestive tract moves slower than normal, the introduction of bacteria species higher up may be bad for you.
What are generally believed to be beneficial probiotic strains may undergo genetic transformation during digestion. Known as horizontal gene transfer, this may result in:
- Friendly probiotic strains may acquire virulence (harmful) factors from pathogens.
- Genetic material changing between the bacterial strains, species, and genera may result in mutated strains being present in your gut flora.
These theoretical dangers of probiotics should be weighed heavily in light of the recent human data on how human gut flora have been confirmed to convert stevia into mutagenic compounds.
By itself, the sweetener is not mutagenic. However after digestion, the bacteria in the intestines create DNA damaging compounds from it. You can read more about this in our analysis for the side effects of stevia.
Do probiotics interfere with antibiotics?
Proponents argue that antibiotics kill off your naturally occurring probiotics and as such, taking them together is beneficial. Opponents argue that the interaction may lead to decreased effectiveness in the prescribed medication.
Given the lack of scientific data to answer this conclusively, it would be best to err on the side of caution and stop taking probiotics while on antibiotics.
Is it safe to take probiotics during pregnancy?
In 2015, the World Allergy Organization recommended probiotics for pregnant women and breastfeeding mothers whose babies are at higher risk for developing allergies. These recommendations “are conditional and supported by very low quality evidence.” They were primarily based on the prevention of eczema and not on evidence that using probiotics will reduce the development of allergies in babies or children. (12)
There have been two published observational studies during the first trimester of pregnancy, with women who were using Lactobacilli probiotics. An increase in malformations was not observed, however these small studies were not designed to specifically examine the pregnancy outcomes. (13) (14)
In a double-blind and placebo controlled study out of Finland involving 256 women, the babies born to mothers using probiotics had a statistically significant lower birth weight and birth length. These were considered desirable because birth size is a risk marker for later obesity. (15)
It has been estimated that the risk of developing bacteremia (bacteria in the blood) from taking Lactobacillus probiotics is less than 1 case per 1,000,000. (16)
The risk of developing fungemia (fungus or yeast in the blood) is estimated to be 1 case per 5,600,000 users and lower in healthy individuals. (17)
Because there is an extremely low risk of mothers developing infections from using probiotic supplements and being that a trend in birth defects or abnormalities has not been observed, it is believed that probiotics are safe for pregnant women to use.
Until there are large-scale clinical trials to carefully monitor usage during the first, second, and third trimesters, as well as the development of the baby after birth, it cannot be conclusively said that probiotics are safe. There may be hidden dangers that have yet to be identified.
Since probiotics would not be expected to be absorbed into the bloodstream, in theory there should be very minimal risk of them being present in breast milk. For that reason, breastfeeding while on probiotics is believed to be safe. Until there is an adequate amount of clinical research to evaluate this, it cannot be said with certainty.
Double-blind trial reports more deaths
Acute pancreatitis is a serious medical condition where there is sudden inflammation of the pancreas.
Due to the release of enzymes and toxins into the bloodstream, it is bad for the heart, lungs, kidneys, and other vital organs.
With proper medical care, 80% of patients recover completely, while the other 20% may suffer permanent organ damage and even death.
On average, around 10% of acute pancreatitis cases result in death, however this number is only 1% when calculating the odds for mild cases. (18)
According to the Mayo Clinic, the causes of acute pancreatitis are (19):
- 45% from gallstones
- 35% from alcohol usage
- 10% are of unknown origin (idiopathic)
- 10% from other, which includes medications, trauma, and surgery
The most severe form of acute pancreatitis is called necrotizing pancreatitis. That’s when there’s a bacterial invasion of the pancreas and it becomes more likely to occur if treatment if delayed.
“These infections are thought to be the sequelae of a cascade of events starting with small-bowel bacterial overgrowth, mucosal barrier failure, and a proinflammatory response leading to bacterial translocation of intestinal bacteria.”
In short, necrotizing pancreatitis is caused by your gut bacteria infecting your pancreas.
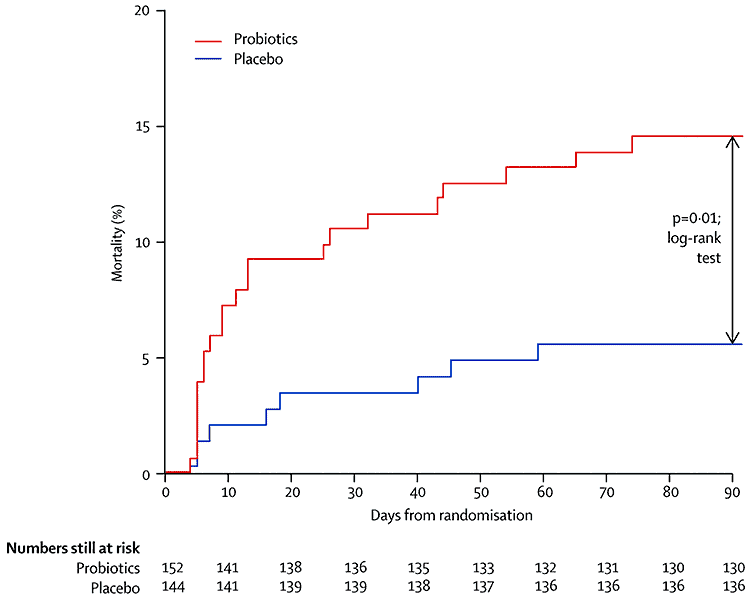
Since antibiotics offer little benefit for treating it, doctors and scientists in the Netherlands wanted to see if probiotics might help. This was a large, multi-center trial and it was published in The Lancet, which is arguably the most respected and prestigious medical journal. (20)
- Randomized, double-blinded, and placebo-controlled
- 298 patients with predicted severe acute pancreatitis participated.
- Within 72 hours of symptoms, they were given either a probiotic (153 patients) or a placebo (145 patients). This was in addition to their standard care.
- Both groups had similar characteristics and disease severity.
The results were alarming and unexpected…
167% more patients died in the probiotics group versus placebo. There were 24 deaths and 9 deaths in each group, respectively.
What makes this even more frightening is how they died. A major cause of death in the probiotics group was not seen whatsoever with placebo:
9 patients in the probiotics group developed bowel ischaemia, which is inflammation and injury of the large intestine result from inadequate blood supply. 8 out of those 9 people died. In the placebo group, there were zero deaths attributed to this.
Are probiotics bad for you?
For people with acute pancreatitis, the clinical data clearly suggests an increased risk of death from using probiotics. In healthy individuals without disease, evidence to date suggests they are safe and may be good for you, though unknown factors remain.
In response to the criticisms about the pancreatitis patients dying, the scientists said that until their study, there was “no doubt about the fact that probiotics were regarded as food supplements with no known side-effects.”
Presumably they meant severe side effects, since milder reactions are common. Regardless, this study shows you how something believed to be perfectly safe may result in unintended and totally unexpected outcomes.
Widespread use of probiotic supplements have really only been within the past two decades and some would argue it’s been even less time than that. Either way, that’s a short time frame in medicine and science.
Just as we don’t understand their full benefits, we need to humbly admit we don’t know their potential dangers. Before we give probiotics to kids and babies with the mindset they’re harmless, we need to admit we don’t know the unknown unknowns, as Donald Rumsfeld might say.
As the authors of the study say, in their conclusion, we need to think of them differently:
“Thus, this combination of probiotics should not be administered routinely in patients with predicted severe pancreatitis, and such preparations can no longer be considered harmless adjuncts to enteral nutrition.”
These statements have not been evaluated by the Food and Drug Administration. This product is not intended to diagnose, treat, cure, or prevent any disease.